Vitamin D is a fat-soluble vitamin that is very important for human health. It not only promotes calcium absorption and is beneficial to bone health, but also plays an important role in improving immunity, improving metabolism, and promoting hormone synthesis.
Many studies in recent years have also found that vitamin D plays an important role in preventing diabetes, reducing the risk of severe respiratory infections, improving the body's chronic inflammatory state, and reducing cardiovascular disease and cancer risks. A new study recently published in the authoritative journal International Journal of Cancer (IJC) also revealed the new "liver protection" effect of vitamin D. Today's article, combined with the latest research results, will talk to you about chronic liver disease patients and vitamin D supplementation.

The liver is an important metabolic and digestive organ in our body, and it is also an important filter for us to decompose harmful substances and remove blood waste. It can be said that liver health is closely related to our overall health. Because our liver is responsible for many important physiological functions, it is also one of the organs most prone to health problems, especially non-alcoholic fatty liver, cirrhosis, hepatitis, liver cancer and other chronic liver diseases, which will cause long-term health hazards to the liver, and may even gradually progress to cirrhosis, hepatocellular carcinoma, etc., and eventually cause liver failure and endanger life.
This new study was published by the research team of Tongji Medical College of Huazhong University of Science and Technology. The study evaluated the correlation between serum vitamin D levels and liver-related diseases. The results showed that adequate serum vitamin D (serum 25-hydroxy D levels) can significantly reduce the risk of various chronic liver diseases.
This study is an observational study based on biobank data. A total of 401,551 participants from the UK Biobank cohort were included in the study. The participants were aged between 37 and 73 years old. All participants had no chronic liver disease when participating in the study, and serum 25-hydroxyvitamin D levels were measured through blood samples. The affinity of the participants' vitamin D binding protein and the activity of the vitamin D receptor were also evaluated.
From the overall serum vitamin D test results, the serum 25-hydroxyvitamin D bark of all participants was lower than 25nmol/L, and the proportion of people with vitamin D deficiency was 12%. Another 42% of the population was vitamin D insufficient (serum 25-vitamin D bark 25 to 50nmol/L), and the serum vitamin D level exceeded 50nmol/L, and the proportion of people reaching sufficient levels was 46%.
The researchers followed up more than 400,000 participants for an average of 15 years. During the follow-up period, a total of 4,404 cases of fatty liver, 1,989 cases of cirrhosis and 480 cases of liver cancer occurred.
The evaluation results show that compared with people with low serum vitamin D levels and vitamin D deficiency, people with sufficient vitamin D levels have a 30% lower risk of fatty liver, a 57% lower risk of cirrhosis, and a 35% lower risk of liver cancer.
In addition to the above three major liver problems, people with sufficient vitamin D also have a similar reduction in the risk of other chronic liver diseases, including alcoholic cirrhosis and liver fibrosis.
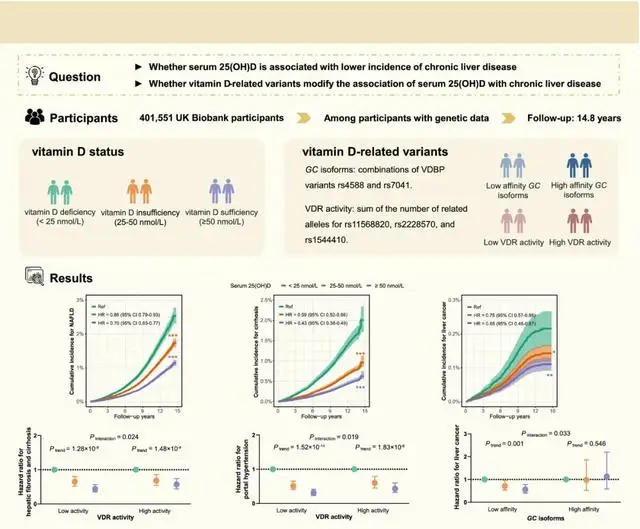
Because the affinity of active vitamin D in serum to vitamin D receptors and the activity of vitamin D receptors vary greatly between different individuals, the researchers also evaluated the association between vitamin D receptor activity and affinity and vitamin D in reducing the risk of chronic liver disease.
The results show that vitamin D receptor affinity and vitamin D receptor activity affect the association between serum active vitamin D and the risk of chronic liver disease. Overall, individuals with low vitamin D receptor activity and poor affinity can maintain adequate vitamin D levels, have a lower risk of chronic liver disease, and have a more significant protective effect on the liver.
That is to say, the poorer the affinity of vitamin D receptors and the lower the activity of vitamin D receptors, the more susceptible liver health is to vitamin D deficiency, and the stronger the protective effect of vitamin D supplementation on the liver is for this group of people.

The specific physiological mechanism of vitamin D's protective effect on the liver is not yet fully understood, but vitamin D can help improve insulin resistance and blood sugar metabolism. This metabolic improvement, in addition to preventing the occurrence of diabetes, also protects the liver's health.
In addition, vitamin D also plays an important role in fighting chronic inflammation, inhibiting cancer cell proliferation, and inducing cancer cell apoptosis. Therefore, supplementing vitamin D can also bring significant benefits to reducing the risk of liver-related cancers.
The significance of this study is that it further reveals the important role of vitamin D in reducing the risk of liver-related diseases, including cirrhosis, liver cancer and other major liver diseases. Statistics show that about 72% of the population in China has vitamin D deficiency or deficiency. For this part of the population, supplementing vitamin D is not only beneficial to enhance immunity and improve bone health, but also has important significance for protecting liver health.

Faced with such research results, how should we supplement vitamin D?
Here are some suggestions for you.
First of all, it is recommended that middle-aged and elderly people should screen their serum 25-hydroxy active vitamin D levels to understand whether they are really deficient in vitamin D. The supplementation strategies we choose may be quite different depending on the deficiency. Moreover, only by understanding the baseline vitamin D situation before supplementation can we better evaluate the supplementation effect after vitamin D supplementation.
Life conditioning supplementation, moderate increase in sun exposure, and eating more vitamin D-rich ingredients, such as deep-sea fish, egg yolks, mushrooms, animal livers, etc., can help supplement the vitamin D level in the body. On this basis, for people with vitamin D deficiency or insufficiency, it is also recommended to choose supplements reasonably.
If you are a person with low vitamin D receptor affinity or poor vitality, you may need a higher dose to supplement vitamin D to achieve sufficient serum active vitamin D levels. However, the specific dose should be determined based on the specific situation and professional evaluation. It is not recommended to supplement vitamin D in large doses for a long time. The daily supplementation dose for long-term supplementation is not recommended to exceed 4000IU.
Ordinary vitamin D3 (cholecalciferol) needs to be converted in the liver and kidneys before it can become active. For cases where the activity of liver vitamin D receptors is low, you can also consider directly supplementing active vitamin D3 or its analogs (such as alfacalcidol), which can bypass the liver's conversion step and work directly.
When taking supplements, grasping the timing of supplementation will also affect the efficiency of vitamin D supplementation. Since vitamin D is fat-soluble, taking it with foods containing healthy fats (such as avocados, nuts, and olive oil) can greatly increase its absorption rate.
Magnesium is an essential cofactor in the metabolism and activation of vitamin D in the body. If you lack magnesium, the effect of supplementing more vitamin D will be greatly reduced. Foods rich in magnesium include green leafy vegetables, nuts, seeds, and whole grains. Therefore, if you want to supplement vitamin D efficiently, confirm whether there is a problem of magnesium deficiency and actively supplement magnesium, which is also an important measure to improve the efficiency of vitamin D supplementation.

Vitamin K2 should also be supplemented. Vitamin K2 is responsible for guiding calcium into the bones instead of depositing it in the blood vessels. When supplementing vitamin D at high doses, adequate vitamin K2 is particularly important to prevent potential risks such as vascular calcification.
For friends who take supplements, strictly follow the doctor's instructions and supplement according to the dosage, and regularly (such as every 3-6 months) review blood indicators to understand the actual effect of vitamin D supplementation, and adjust the supplementation plan in time according to the situation.
I hope that everyone can correctly understand the important relationship between vitamin D supplementation and liver health.

%20--%3e%3c!DOCTYPE%20svg%20PUBLIC%20'-//W3C//DTD%20SVG%201.1//EN'%20'http://www.w3.org/Graphics/SVG/1.1/DTD/svg11.dtd'%3e%3csvg%20version='1.1'%20id='图层_1'%20xmlns='http://www.w3.org/2000/svg'%20xmlns:xlink='http://www.w3.org/1999/xlink'%20x='0px'%20y='0px'%20width='256px'%20height='256px'%20viewBox='0%200%20256%20256'%20enable-background='new%200%200%20256%20256'%20xml:space='preserve'%3e%3cpath%20fill='%23FFFFFF'%20d='M194.597,24.009h35.292l-77.094,88.082l90.697,119.881h-71.021l-55.607-72.668L53.229,232.01H17.92%20l82.469-94.227L13.349,24.009h72.813l50.286,66.45l58.148-66.469V24.009z%20M182.217,210.889h19.566L75.538,44.014H54.583%20L182.217,210.889z'/%3e%3c/svg%3e)